ABSTRACT
Background: The adult lifetime incidence for low back pain is 75% to 85% in the United States. Investigating appropriate care has proven difficult, since, in general, acute pain subsides spontaneously and chronic pain is resistant to intervention. Subacute back pain has been rarely studied.
Objective: To compare the relative efficacy of chiropractic adjustments with muscle relaxants and placebo/sham for subacute low back pain.
Design: A randomized, double-blind clinical trial.
Methods: Subjects (N = 192) experiencing low back pain of 2 to 6 weeks’ duration were randomly allocated to 3groups with interventions applied over 2 weeks. Interventions were either chiropractic adjustments with placebo medicine, muscle relaxants with sham adjustments, or placebo medicine with sham adjustments. Visual Analog Scale
for Pain, Oswestry Disability Questionnaire, and Modified Zung Depression Scale were assessed at baseline, 2 weeks,and 4 weeks. Schober’s flexibility test, acetaminophen usage, and Global Impression of Severity Scale (GIS), a physician’s clinical impression used as a secondary outcome, were assessed at baseline and 2 weeks.
Results: Baseline values, except GIS, were similar for all groups. When all subjects completing the protocol were combined (N = 146), the data revealed pain, disability, depression, and GIS decreased significantly (P < .0001); lumbar flexibility did not change. Statistical differences across groups were seen for pain, a primary outcome, (chiropractic group improved more than control group) and GIS (chiropractic group improved more than other groups). No significant differences were seen for disability, depression, flexibility, or acetaminophen usage across groups.
Conclusion: Chiropractic was more beneficial than placebo in reducing pain and more beneficial than either placebo or muscle relaxants in reducing GIS.
(J Manipulative Physiol Ther 2004;27:388-98) Key Indexing Terms: Chiropractic; Central Muscle Relaxants; Low Back Pain; Randomized Controlled Trial
INTRODUCTION
Low back pain (LBP) has an adult lifetime incidence
of 75% to 85% in the United States, with a yearly
prevalence of 15% to 20%. 1-3 Common classifica-
tions, based on pain duration, include acute (2 weeks or
less), subacute (2 to 12 weeks), and chronic (more than 12
weeks). Some studies have shown subacute pain to have
clinical characteristics similar to acute LBP. 4,5 While acute
pain usually subsides spontaneously, chronic pain is gener-
ally resistant to intervention 1,2,6-8 and often becomes a
recurrent problem. 6
The Agency for Health Care Policy and Research
(AHCPR) noted that nonsteroidal anti-inflammatory com-
pounds and muscle relaxants were effective for the pain
component of low back proble ms .9 Spinal manipulation
was found to be effective for functional recovery and was
recommended for uncomplicated acute LBP within the first
month of symptoms. Other reviewers found evidence to
support spinal manipulation for acute LBP, resulting in both
short-term benefits 10-14 and long-term benefits of 1 to 3
years. 15-17 Giles and Muller 18 and Hsieh et al 19 concluded
that chronic LBP patients benefit from chiropractic adjust-
ments. In a systematic revie w of conservative interventions
for subacute low back pain, Pengel et al 20 concluded there is a
major gap in the evidence for inte rventions that are recom-
mended in current clinical guidelines.
Reviews of LBP studies 10,12,14,15,21 often fail to distin-
guish between manipulative interventions. Manipulation
and spinal manipulative therapy (SMT) are vague terms
describing procedures used by chiropractors, physiothera-
pists, massage therapists, and osteopaths. These maneuvers
may decrease ligamentous adhesions and myospasm, in-
crease disk nutrition, or alter the function of the nervous
system. The manipulative procedures used in this study,
referred to as chiropractic a djustments, involve specific
application of force thought to restore mechanical and
neurological function to the spine. 22-24
Routine chiropractic care generally involves adjusting
multiple areas of the spine, as indicated through spinal
evaluation 25,26 This is supported by Nyiendo et al 27
in studies of patients suffering chronic, recurrent low back
pain. Those patients seeing chiropractors were more likely
(61%) to receive full spine adjustment and less likely (39%)
to receive adjustment only at the site of pain (lumbopelvic
region). Further, in a study of 12 chiropractors who
specialized i n only performing upper cervical specifi c
adjustments, 28% of new patients presented with low back
pain.28
One explanation for this is that even though the
lumbar facets or sacroiliac articulations may generate the
primary pain symptom, the primary dysfunction may be
found in other areas of the spine, and it has been proposed
that central neurological mechanisms may play an important
role. 29-31 Arkuszewski 32 supports the involvement of the
cervical spine in back pain and the influence of manual
treatment of the cervical segments on different signs of
dysfunction of the locomotor system. In 100 patients with
lumbar pain or sciatica, 60% had concomitant neck pain.
Cervical dysfunction was found at the atlanto-occipital
segments in 95% of these patients.
Although chiropractic care has fared well in comparison
studies, 14,21no study has directly compared chiropractic
adjustments with muscle relaxants. Andersson et al 33
demonstrated subjects with 3 weeks to 6 months of LBP
responded equally well to osteopathic spinal manipulation
or standard medical care. A muscle relaxant, cyclobenza-
prine, was an option of care, but its effect could not be
isolated, since a minority of subjects in both treatment
groups received the drug.
This study met approval of the Life University institu-
tional review committee. The goal of this trial was to study a
specific classification of subacute LBP, comparing chiro-
practic adjustments with m uscle relaxants a nd placebo,
using an intervention phase typical of drug therapy.
METHODS
Randomization and Blinding
This study was a randomized clinical trial (RCT) in
which subjects and assessors were blinded to the inter-
ventions, chiropractic providers were blinded to medical/
sham assignment, and an independent consultant provided
the statistical analysis. Visit lengths and provider-subject
interactions were monitored to preserve patient blinding.
Subjects were assigned sequential enrollment numbers that
provided group assignment based on a computer-generated
randomization chart.
Subject Selection
Advertisements were used to recruit subjects, 21 to 59
years old, with uncomplicated LBP of 2 to 6 weeks
duration. Exclusion criteria included previous spinal sur-
gery, sp inal fractures, spinal sten osis, and known or
suspected disk herniation; previous LBP within 18
months; neuropathy; spondylitis; vascular disease; malig-
nant disease; cervical complaint; pregnancy; and personal
injury litigation. Following infor med consent procedures,
eligibility was established jointly by doctors of chiro-
practic and medicine through history taking and a physi-
cal examination.
Criteria for Chiropractic Adjustment
Chiropractic assessment.
A chiropractic examination at the initial visit ascertained the
presence and nature of spinalmisalignments. The assessment
of the spine included palpation of joints and muscles to assess
range and resistance of joint motion, as well as level of tenderness
and/or presence of inflammation. 34-37
Radiographic examination.Radiographic procedures were
performed on the first visit. Those patients assigned to
the chiropractic care group received 6 radiographs: late ral
cervical, verte x, 2 nasium cervical views (before and after
first chiropractic adjustment), and anterior-to-posterior and
lateral lumbopelvic. The films were used for chiropractic
radiographic analys is to provide specific spinal adjust-
ments. Radiation exposure was minimized through high-
frequency equipment, high-speed film, rare earth screens,
lead filters, and shielding.
Sham radiographic examination.Participants in the medical and
control groups were positioned so as to receive each of the 6
radiographs, but no exposures were made.
Interventions
Subjects were randomly assigned to 1 of 3 groups: (1)
chiropractic adjustments and medical placebo, (2) muscle
relaxants and sham adjustments, and (3) medical placeb o
and sham adjustment. Al l subjects received acetaminophen
as a ‘‘rescue medication’’ to allow assessment of self-
medication. Subjects attended 7 chiropractic visits and
self-administered medication/placebo capsules over
2 weeks.
Chiropractic adjustments.At each visi t, the chiropractic care
that was provided was tailored to each subject’s needs and
included both upper cervical and lumbar, sacral, or pelvic
adjustments. 34-37 Manual spinal adjustments were per-
formed on a drop table (equipped with sections that could
travel a limited excursion once a preset load was exceeded),
with the subject in either a prone or side- lying position using
specific, high-velocity, low-amplitude thrusts in the lumbar,
pelvic, or sacral spinal region. 36
Supine leg length inequality (LLI) and adjustment vectors were
determined according to the Grostic Procedure. 34,35,38,39
The subject was placed in a side-lying position with the head
resting on the mastoid process. Using a handheld instrument
(KME Enterprises, Atlanta, Ga) with an electromagnetically driven
stylus, a high-velocity, limited excursion thrust was delivered along
a lateral- to-medial vector with skin surface contact over the level
of the atlas (C1 vertebra) transverse process.
Sham procedures.Sham procedures were designed to mimic
chiro practic adjustments with resp ect to dialogue, visit
length, and physical contact. For lower spine sham pro-
cedures, the subject was placed prone on a drop table with the
lumbar and pelvic sections activated (lifted but not released)
or alternatively, in a side-lying (semifetal) position on a
bench. The chiropractor’s hand was placed over the para-
vertebral musculature and light pressure was applied. Caution
was taken to avoid an actual thrust to the spine. For the
cervical sham procedures, the subject was placed in a supine
position and the adjusting instrument was positioned over the
mastoid. The instrument was disabled so that no thrust was
delivered to the spinal articulations.
Drug therapy.The use of muscle relaxants is common in
medical practice for treating back pain, and both nonsteroi-
dal anti-inflammatory compounds and muscle relaxants
were noted as effective for the pain component of low back
problems by the AHCPR. 9 The 3 agents used in this study
(cyclobenzaprine HCl, 5 mg; carisoprodol, 350 mg;
methocarbamol, 750 mg) and their usage instructions were
chosen by the medical doctor based on his own clinical
experience and were designed to mimic general medical
care with a 2-week duration. The medications affect motor
activity through central mechanisms. Cyclobenzaprine HCl
reduces tonic somatic motor activity primarily within the
central nervous system. Carisoprodol has been shown to
produce muscle relax ation in animals by blocking interneu-
ronal activity in the descending reticular formation a nd the
spinal cord. Methocarbamol is thought to depres s the central
nervous system. 40
The medical doctor dispensed medication kits that
contained 4 bottles. Subjects in the medical group were
given 3 muscle relaxants in bottles labeled A, B, and C.
Subjects were given written and verbal instructions referring
to bottles by letter only. Subjects were instructed to record
on a medication log the amount of each drug used and any
side effects encountered.
The initial dose was 2 capsules at bedtime from bottle A
and 2 capsules, 3 times daily from bottle B. Medication
from bottles A and B could be doubled or halved as needed.
If subjec ts expe rienced ex cessive side effects s uch as
drowsiness or sleeplessness from a medicine, they wer e
allowed to substitute bottle B for A and bottle C for B, again
doubling or halving dosages as necessary. If excessive side
effects continued after switching to bottle C, instructions
were to stop taking all capsules. Subjects were informed that
bottle D contained acetaminophen (500 mg), and the max-
imum dose was 2 capsules, 3 times daily.
Placebo drug therapy.There was no visual difference between
the medication and corresponding placebos. Bottles labeled
A, B, and C given to the control and chiropractic groups
contained capsules filled with an inactive placebo; bottle D
contained acetaminophen tablets. Subjects in the chiroprac-
tic and control groups received instructions identical to
those of the medical group.
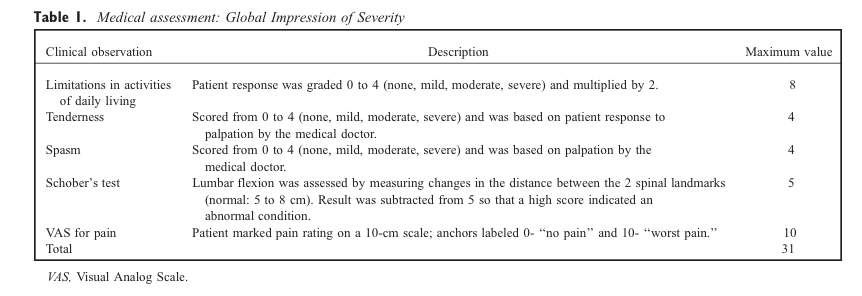
Outcome Assessments
After a series of meetings between 1993 and 1997, a
World Health Organization informal committee recommen-
ded 4 primary outcome measures for clinical trials investi-
gating low back pain. 4 Three valid and reliable measures, a
Visual Analog Scale (VAS) for Pa in, 42-44 the (original)
Oswestry Low B ack Pain Disability Questionnaire, 45-47
and the Modi fied Zung Self-Rating for De pression
Scale, 48-51 were administered at the initial visit (baseline)
and repeated at 2 weeks and 4 weeks. A fourth measure,
Schober’s test, was done at baseline and 2 weeks to
evaluate lumbar flexibility. 52,53 Two secondary outcome
measures were used: acetaminophen usage during the 14-
day intervention phase and a final measure, termed Global
Impression of Severity (GIS), which was implemented in
the study to determine its usefulness in assessing temporal
aspects of physical examination findings. GIS scores ranged
from 0 to 31 and were derived by combining 5 measures
determined by a medical doctor performing a blinde d
evaluation (Table 1).
Statistical Analysis
The statistical analysis was designed by a doctorate-level
biostatistician from an indepe ndent university. The initial
analysis confirmed the normality of outcome measures at
each asses sment, lending to param etric methods for signif-
icance testing. Subjects were analyzed in the intervention
group to which they were randomized (intent-to-treat), but
to eliminate erroneous assumptions made for missing data
points, data for each outcome measure were restricted to
subjects who completed the assessments.
A general linear model analysis of variance (ANOVA)
was used for outcome measures looking for a significant
time by intervention group interaction ( P < .05). If groups
differentially changed over time, familywise comparisons
were made using the Tukey Honestly Significant Differ-
ence (HSD) studentized range tests, which control for type
1 error.
RESULTS
Subject Recruitment and Follow-Up
The various recruiting methods used for this study
resulted in 2570 inquiries. Most people responded to adver-
tisements or public service announcements from newspapers
(1897), radio (98), television (82), magazines (72), or an
Internet posting (1). Of the remainder, 89 persons were
referrals, and 331 did not recall the advertising source.
Subsequent telephone interviews screened prospective
participants based on rigid inclusion criteria. The majority
of the subjects (79.2%) failed to qualify for 1 or more
reasons. The most common reason for excluding subjects
was because their LBP duration was too long (chronic) or
the pain pattern was judged recurrent. Other main reasons
for exclusion included known or suspec ted cause of LBP
and recent care for the condition. Of the 535 subjects who
were eligible based on the telephone interview, ab out half
(246) were sufficiently interested to be scheduled to receive
a history and examination by the medical/chiropractic team
to determine second-stage eligibility. Of these, 20 failed to
show up for their initial appointment and were dropped from
the study. Of the subjects that received an examination, 34
of pain (18), current medication usage (3), presence of neck
pain (2), no time commitment by subject (4), pain duration
outside of the 2- to 6-week window (4), recurrent pain (1),
no present pain (1), and breast-feeding (1) (contraindicat ion
to use of radiographs). The remaining 192 subjects were
enrolled in the study and randomly assigned to 1 of 3 groups
receiving chiropractic, medi cal, or no care with appropriate
sham/placebo procedures employed to maintain s ubject
blinding to group assignment.
Once enrolled in the study, patient retention was good. Of
the 192 subjects who were enrolled in the study, 159
(82.8%) comp leted the 2-week care phase a nd 146
(76.0%) returned 2 weeks thereafter for final data collection.
There was no group bias for dropouts (chiropractic 13,
medical 17, control 13; m 2 analysis, P = .75), and most
subjects dropped out due to time constraints. Data from 3
subjects were discarded because 2 had initiated personal
injury litigation (an exclusion criterion) and another inad-
vertently received both forms of active intervention.
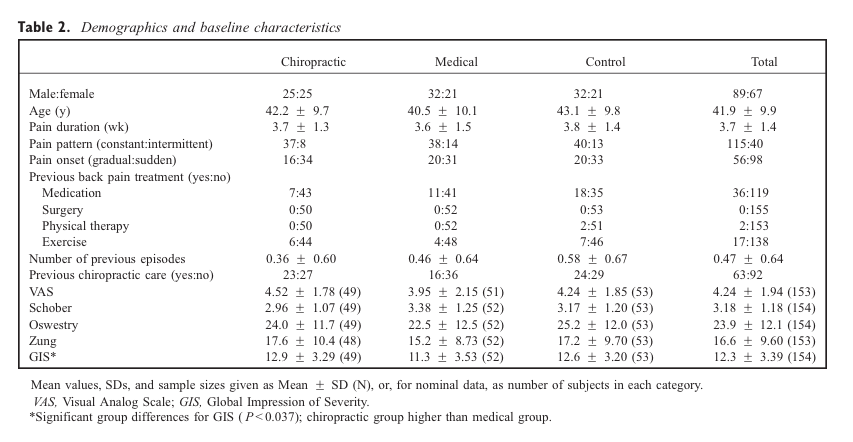
Demographics
Randomization resulted in similar groups (Table 2),
except for initial GIS scores. The mean F SD for age and
pain duration were 41.9 F 9.9 years and 3.7 F 1.4 weeks.
Most subjects had constant pain and two thirds had sudden
rather than gradual onset of pain. Based on a ‘‘yes’’ or ‘‘no’’
response to the telephone interview question, ‘‘Have you
ever had any prior episodes of low back pain?,’’ the majority
of subjects (60%) report ed they were experiencing their first
episode of LBP lasting longer than 2 weeks, and in addition,
all subjects reported ‘‘no’’ to an interview question regard-
ing whether they had received any treatment for low back
pain for the current episode.
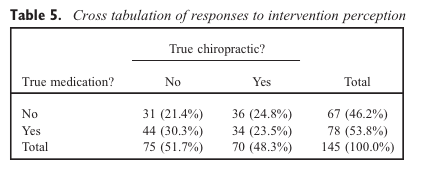
Blinding
To help assess the success of blinding as to assignment to
treatment group, subjects were asked at the end of the study
whether they thought they received true chiropractic adjust-
ments and true medications. Tables 3 and 4 list the results of
these 2 questions based on group assignment. Subjects had
an equal likelihood of being placed in any of the 3
intervention groups. If subjects understood the experimental
design and were successfully blinded to the interventions
used, one would expect about one third of the subjects to
say they received actual care. This was not the case, and m
2 analysis revealed significant cross-group differences to both
questions (chiropractic adjustments: P < .001; medications:
P = .008). Follow-up pair-wise comparisons revealed that
perception of true chiropractic care was significantly higher
( P < .05) in the chiropractic group than either of the other
2 groups, as might be predicted if the sham maneuver did
not closely approximate the true adjustment. However,
significantly more subjects in the medical group perceived
receiving true chiropractic care than in the control group, a
result that is difficult to interpret. When respondin g to
whether they received true medication, response patterns
were similar in the medical and control groups, but both of
these had significantly higher positive response rates than
the chiropractic group.
Table 5 compares response rates to the 2 questions
regarding perception of true care. About the same number
of subjects fit into each of the 4 potential response combi-
nations (no/no, no/yes, yes/no, yes/yes), even though the
study design did not allow subjects to receive both active
forms of intervention.
Subject Compliance
The 2-week care phase involved a total of 8 visits over a
2-week period, which was followed by a ninth visit 2 weeks
thereafter for a final assessment. The majority of the subject
pool that completed the care phase attended all 8 scheduled
visits (N = 154, m ean = 7.68, SD = 0. 72). T here was no
difference in the number of visits across intervention groups.
On completion of the care phase, subjects were asked to
return their medication kits along with their completed
medication logs. A total of 126 people (82%) retur ned
their medication kits and 121 people (79%) returned their
medication logs. Turning in kits was moderately associated
with turning in logs: 83% of subjects turned in both or
neither, kappa = 0.49. Out of concern that medication
usage data were biased toward certain types of subje cts, a
series of t tests was performed looking for differences in
the 2 groups of subjects who did or did not fill out their
medication logs. There was no statistical difference be-
tween these groups for baseline values of VAS for Pain,
Oswestry Low Back Pain Disability Questionnaire, Mod-
ified Zung Self-Rating for Depression Scale, or Schober’s
test, implying that subjects who provided medication usage
data were representative of the entire subject pool.
Medication/placebo usage was appraised from the logs
and the bottle counts. Both methods are prone to error;
subjects might have forgetten to update their logs when
taking medication, and subjects might have taken pills out
of the containers without actuall y ingesting them. Both
result in higher bottle counts relative to log counts, and
the data indicate bottle counts for all 4 pills combined were,
on average, 24.9 pills higher than the log counts. However,
there were no usage differences across groups.
In summary, subjects in the 3 intervention groups re-
ceived the same number of chiropractic procedures (real or
sham) and the same number of pills (medication or placebo).
The amount of acetaminophen taken (bottle D) is described
below in Secondary Outcome Measures.
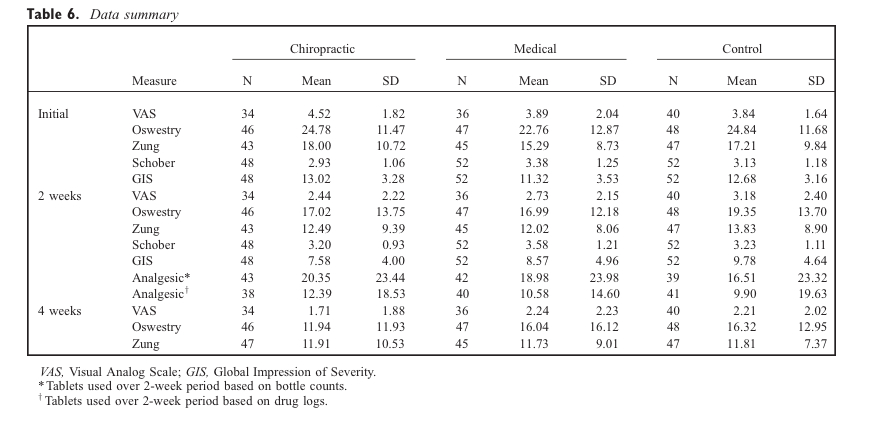
Primary Outcome Measures
Table 6 lists summary data for all outcome measures.
Visual Analog Scale for Pain. The 4-week VAS was not
assessed during a portion of the study due to administra-
tive error.
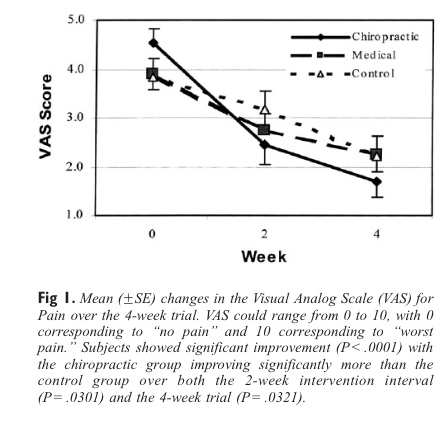
ANOVA for all subjects combined showed a signifi-
cant decrease in pain (see Fig 1) over the 4-week trial
( P < .0001). Mean baseline values for VAS were higher for
the chiropractic group (16% and 18% higher than the
medical and control groups, respectively) and final values
were lower for the chiropractic group (24% and 23%), but
none of these differences were statistically significant.
However, ANOVA did reveal that the change in reported
pain during the trial did vary among intervention groups, a
result that was significant ( P = .0321). Post hoc analysis
revealed that subjects in the chiropractic group reported
greater pain reduction than the control group. Similar
findings were seen during the 2-week intervention phase,
where there was also a significant difference in change
scores across groups ( P = .0301) and the chiropractic group
improved more than the control group ( P < .05).
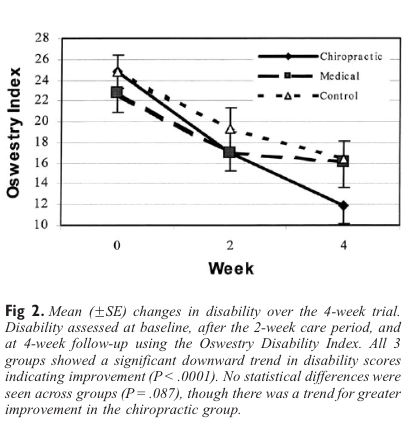
Oswestry Disability Index.Figure 2 reveals a significant decline
in disability for all groups ( P < .0001) with the greatest
decline occurring in the chiropractic care group, though it
was not significantly different ( P = .087).
Modified Zung.As shown in Figure 3, depression scores
improved significantly over the course of the study for all
groups ( P < .0001). However, there were no significant
differences among the groups ( P = .319).
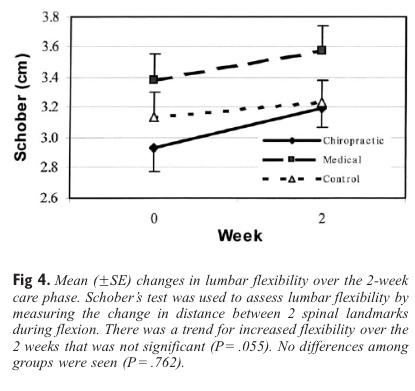
Schober’s test.Figure 4 displays a modest, but insignificant,
increase in flexibility for combined groups ( P = .055); there
were no differences among the groups ( P = .762).
Secondary Outcome Measures
Acetaminophen usage.
The use of acetaminophen was calculated throu gh remaining pill
counts and medication logs. Moderate usage of 1.33 F 1.67 capsules
per day
logs was demonstrated. There was no statistical difference
across groups in the number of tablets taken calculated by
bottle counts ( P = .760) or by logs ( P = .814).
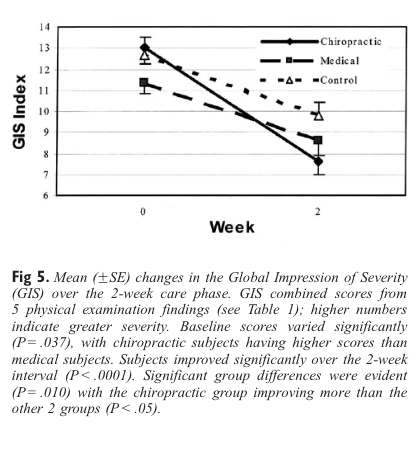
Global Impression of Severity. Figure 5 shows a significant
decline in GIS for all groups ( P < .0001) and significant
differences among groups ( P = .010). Post hoc analys is
revealed the chiropractic group improved significantly more
than both other groups ( P < .05).
DISCUSSION
In all groups, for each outcome measure, there was
improvement after 2 week s of care and further improvement
at the 4-week follow-up, so these subacute subjects appear
to improve in a manner similar to acute pain sufferers.
4,5 The improvements in the placebo group likely represent
natural history.
After the 2-week intervention phase, chiropractic adjust-
ments were shown to be statistically more beneficial than
placebo in reducing pain and more beneficial than placebo
or muscle relaxants in reducing GIS; however, there were no
differences across groups for disability. For the disability
measure, post hoc analysis revealed the power of the present
study to be 59%. Further, a ssuming means and variances
seen in the present study and a power level of 80%,
increasing the sample population to 72 subjects per group
could have yielded significant advanta ges for chiropractic
adjustments. No group differences were seen with the
Modified Zung, as would be expected since depression is
mild during the acute/subacute phase, nor were differences
observed for flexibility or analgesic usage.
Previous comparisons of SMT to medical care for LBP
have shown mixed results. A study of subjects with 3 to 26
weeks of LBP showed no additional benefit for osteopathic
manipulation over standard medical care, which included
medicines and physical modality. 33 Similarly, a study of
acute LBP showed manipulative physiotherapy was no more
beneficial than nonsteroidal anti-inflammatory drugs
(NSAIDs). 54In chronic LBP, no group differences were
seen for trunk-strengt heni ng exercises supplemented b y
either chiropractic manipulation or NSAIDs.55 Conversely,
other chronic spinal pain studies have shown spinal manip-
ulative procedures more beneficial than NSAIDs 18 and
spinal manipulation more beneficial than continued care
using analgesics and NSAIDs. 15 In light of the differing
methodologies ac ross studies, it is difficult to draw any
strong conclusions.
In this study, care was restricted to 2 weeks, although in
practice, chiropractors typically see patients for longer
periods. Other trials comparing chiropractic adjustments to
medical care for LBP allowed for 9 visits over 1 month, 56
10 treatments over 1 year, 16 or, in a childhood asthma study,
20 to 36 visits over 4 months. 57 Though improvement was
marked and rapid in the present trial, providing the chiro-
practors with more latitude in their care plan might
have provided additional benefit. As follow-up extended
only to 4 weeks, long-term benefits of the interventions
are unknown.
Outcomes in randomized drug therapy trials often in-
clude assessment of global improvement and 5 specific
domains of back pain: local pain, muscle spasm , range of
motion, tenderness to palpation, and activities of daily
living. 58
The GIS used in this study has not been tested
for reliability and validity and is subjective by its very
cance. The measure did provide a broadly based assess-
ment, was normally distributed, demonstrated a useful
range, and was responsive to 2 weeks of intervention/time.
In a clinical perspective, the severity of a patient presenting
for care is often subjectively rated. In this study, the GIS
represented a blin ded evaluation of severity by the medical
doctor using his own scoring method. There was overlap in
outcome assessments, since GIS was formed from 5 mea-
sures, 2 of which were analyzed individually. However,
analysis of GIS data without the VAS or Schober’s com-
ponents did not change the results. The GIS showed that
subjects given chiropractic adjustme nts and placebo medi-
cine improved more than subjects who received placebo
medicine or muscle relaxants did (in combination with
sham adjustments). However, it should be noted that the
chiropractic group mean was worse at baseline, giving a
slightly more favorable adv antage toward improvement
based solely on natural history.
In this study population, only modest changes in flexi-
bility were seen and no difference among groups emerged
using Schober’s test. The reliability and validity of Schob-
er’s test for testing lumbar flexibil ity have been debated.
Researchers have found Schober’s test works as well as the
computerized CA-6000 Spinal Motion Analyzer (Ortho-
pedic Systems Inc, Union City, Calif) in assessing lumbar
flexion and that a modified Sch ober test is superior to
double inclinometer methods for flexion, while another
study suggests use of a modified Schober could introduce
systematic errors and its use is questionable.
59-61
Although lifetime usage figures are not available, approxi-
mately 7% to 10% of the overall population uses chiropractic
in a given year. 62,63 The study population was not naı¨ve to
chiropractic interventions. Since 40% also reported previous
LBP (exclusion criteria: occurrence >18 months prior), it is
not surprising to find a 41% lifetime history of chiropractic
care (exclusion: occurrence >18 months prior). Even so, the
post hoc analysis found no significant association of previous
chiropractic care with blinding, dropout rate, or changes in
VAS for pain.
Although blinding procedures directed toward the pro-
viders and assessors were successful, whether subjects
remained blinded is debatable. A high percentage of subjects
in the chiropractic and medical groups responded correctly to
questions regarding the intervention received. This is not
unusual in clinical trials, since many interventions deliver a
powerful and readily apparent effect. However, it is difficult
to interpret why statistically more control subjects than
chiropractic subjects in this study thought they were receiving
true medications. It would seem that the blinding procedures
used here were no less successful than those used in other
rigorous randomized clinical trials. 56,57,64
Blinded, randomized clinical trials are considered the gold
standard of e xperim ental de sign. 9,15,21,65
Yet, blinding remains elusive in studies where the intervention
may be invasive (eg , surgery, acupuncture) or involve physical
contact between the subject and the care provider (eg,
chiropractic, osteopathy, massage). An appropriate chiro-
practic sham p rocedure requires a maneuver that makes
subjects think they are getting a spinal adjustment without
actually causing osseous rearrangement. Joint cavitation
commonly occurs during activities that approach endpoint
range of motion, and this may cause changes in the spine.
Joint cavitation was noted twice in the present study during
lumbar sham procedures. Even well-designed sham proce-
dures could cause inadvertent correction. Further, there is
the po ssibility that palpation of spastic paraspinal muscles
and other contiguous tissues may cause spinal changes.
Thus, previous rigorous sham-controlled studies in chiro-
practic that demonstrated global benefits to all intervention
groups while failing to show differential benefits 57 may
have been inadvertently providing benefit to the control group.
Study Limitations
In a factorial design, a fourth group could have been
randomized to receive both active interventions. Further-
more, this study did not provi de for a 1-year follow-up.
Possibly, long-term follow-up could help to identify differ-
ent recovery patterns in these groups. Stratification on the
study population for the wide ranges in pain and disability
scores (large SD) in a separate analysis may provide
characteristics of responders versus nonresponders for both
types of interventions.
Health care providers often rate the severity of present-
ing complaints of patients using subjective means. The
GIS used for a blinded assessment by the medical physi-
cian needs to be tested for reliability and validity; there-
fore, the significance of the results for GIS should be
interpreted cautiously.
Increasing the sample size according to power analysis,
lengthening the care phase to 6 weeks to provide care more
in line with practice standards, and providing a 1-year
follow-up would improve future studies.
CONCLUSION
This study identified a sample population of subacute
low back pain sufferers for which chiropractic care provid-
ed an equally effective management to the conservative
medical care of muscle relaxants. However, as subjects
responded well to time (and placebo), these design changes
may not provide the strong clinical evidence needed to
recommend a particular intervention for management of
subacute back pain.
Statistically, the chiropractic group responded signifi-
cantly better than the control group with respect to a
decrease in pain scores.
ACKNOWLEDGMENTS
We extend sincere appreciation to Life University for
providing funding and clinical facilities. We are grateful for
many contributions: Medhat Alattar, MBBCh, MS, DC,
George Erhlich, MD, and Edward F. Owens, MS, DC for
assistance in design; Susan Brown , PhD, DC and Scott
Clark, PhD for statistical assistance; Mark White, DC and
Hayes Wilson, MD for patient care; Cathy Crowley, RPh for
pharmaceutical assistance; Research Faculty, Staff, and
Students and Clinic Faculty for technical assistance; Charles
(Skip) Lantz, PhD, DC and Virginia Q. Kaderabek, BA for
reviewing and editing the manuscript. We would like to
acknowledge the contributions of the late John D. Grostic,
DC in the early developmental stages.
Bruce Pfleger, PhD, (b)
George Cotsonis, MA, (d)
Omar Elsangak, MBBCh, DC, (e)
Roger Hinson, DC, (f)
and Gregoria T. Verzosa, DC (g)
1. Allan DB, Waddell G. An historical perspective on low back
pain and disability. Acta Orthop Scand 1989;60:1-23.
2. Andersson GBJ. Epidemiology of low back pain. Acta Orthop
Scand 1998;69(Suppl 281):28-31.
3. Waddell G. Low back pain: a twentieth century health care
enigma. Spine 1996;21:2820-5.
4. Linton SJ, Hallden K. Can we screen for problematic back
pain? A screening questionnaire f or predicting outcome in
acute and subacute back pain. Clin J Pain 1998;14:209-15.
5. Sinclair SJ, Hogg-Johnson S, Mondloch MV, Shields SA. The
effectiveness of an early active intervention program for work-
ers with soft-tissue injuries: the early claimant cohort study.
Spine 1997;22:2919-31.
6. Carey TS, Garrett J, Jac kman A, McLaughlin C, Fryer J ,
Smucker DR. The outcomes and costs of care for acute low
back pain among patients seen by primary care practitioners,
chiropractors, and orthopaedic surgeons. N Engl J Med 1995;
333:913.
7. Deyo RA, Phillips WR. Low back pain. A primary care chal-
lenge. Spine 1996;21:2826-32.
8. Von Korff M, Saunders K. The course of back pain in primary
care. Spine 1996;21:2833-9.
9.BigosSJ,BowyerOR,BraenGR,BrownKC,DeyoRA,
Haldeman S, et al. Acute low back pain problems in adults.
Clinical practice guideline no. 14. Rockville (MD): Agency
for Health Care Policy and Research; 1994 (AHCPR publica-
tion 95-0642).
10. Abenhaim L, Bergeron AM. Twenty years of randomized clini-
cal trials of manipulative therapy for back pain: a review. Clin
Invest Med 1992;15:527-35.
11. Haldeman S. Spinal manipulative therapy in sports medicine.
Clin Sports Med 1986;5:277-93.
12. Moritz U. Evaluation of manipulation and other manual ther-
apy. Criteria for measuring the effect of treatment. Scand J
Rehabil Med 1979;11:173-9.
13. Raftis KL, Warfield CA. Spinal manipulation for back pain.Hosp Pract (Off Ed) 1989;24:89-90, 95-6, 102.
14. Shekelle PG, Adams AH, Chassin MR, Hurwitz EL, BrookRH. Spinal manipulation for low back pain. Ann Intern Med1992;117:590-8.
15. Koes BW, Bouter LM, van Mameren H, Essers AH, Verste-gen GM, Hofhuizen DM, et al. The effectiveness of manualtherapy, physiotherapy, and treatment by the general practi-tioner for nonspecific back and neck complaints. Spine 1992;17:28-35.
16. Meade TW, Dyer S, Browne W, Townsend J, Frank AO. Lowback pain of mechanical origin: randomized comparison ofchiropractic and hospital outpatient t reatment. BMJ 1990;300:1431-7.
17. Meade TW, Dyer S, Browne W, Frank AO. Randomized com-parison of chiropractic and hospital outpatient management forlow back pain: results from extended follow-up. BMJ 1995;311:349-51.
18. Giles LG, Muller R. Chronic spinal pain syndromes: a clini-cal pilot trial comparing acupuncture, a nonsteroidal anti-inflammatory drug, and spinal manipulation. J ManipulativePhysiol Ther 1999;22:376-81.
19. Hsieh CY, Phillips RB, Adams AH, Pope MH. Functionaloutcomes of low back pain: comparison of four treatmentgroups in a randomized controlled trial. J Manipulative Phys-iol Ther 1992;15:4-9.
20. Pengel HM, Maher CG, Refshauge KM. Systematic review ofconservative interventions for subacute low back pain. ClinRehabil 2002;16:811-20.
21. Anderson R, Meeker WC, Wirick BE, Mootz RD, Kirk DH,Adams A. A meta-analysis of clinical trials of spinal manipu-lation. J Manipulative Physiol Ther 1992;15:181-94.
22. Gatterman MI. What’s in a word? In: Gatterman MI, editor.Foundations of chiropractic: subluxation. St. Louis: Mosby-Year Book; 1995. p. 5-17.
23. Janse J. History of the development of chiropractic concepts:chiropractic terminology. In: Goldstein M, editor. The re-search status of spinal manipulative therapy. US Depart-ment of Health, Education, and Welfare. Bethesda (MD):Public Health Service; 1975. p. 25-42 (National Institutesof Health NINCDS Monograph 15).
24. Leach RA. Manipulation terminology. In: Leach RA, editor.The chiropractic theories: principles and clinical applications.3rd ed. Baltimore: Williams and Wilkins; 1994. p. 15-22.
25. Meeker WC, Haldeman S. Chiropractic: a profession at thecrossroads of mainstream and alternative medicine. Ann InternMed 2002;136:216-27.
26. Christensen MG, Kerkoff D, Kallasch MW. Job analysis ofchiropractic. A pr oject report, survey analysis and summaryof the practice of chiropractic within t he United State s.Greeley (CO): National Board of Chiropractic Examiners;2000. p. 115-7.
27. Nyiendo J, Haas M, Goodwin P. Patient characteristics, prac-tice activities, and one-month outcomes for chronic, recurrentlow-back pain treated by chiropractors and family medicinephysicians: a practice-based feasibility study. J ManipulativePhysiol Ther 2000;23:239-45.
28. Hoiriis KT, Owens EF. Changes in general health status duringupper cervical chiropractic care: a practice-based researchproject update. Chiropr Res J 1999;6:65-70.
29. Henderson C. Three neurophysiologic theories on the chiro-practic subluxation. In: Gatterman MI, editor. Foundations ofchiropractic: subluxation. St. Louis: Mosby; 1995. p. 225-33.
30. Lantz C. The vertebral subluxation complex. In: Gatterman M,editor. Foundations of chiropractic: subluxation. St. Louis:Mosby; 1995. p. 149-74.
31. Miller KE, Douglas VD, Richards AB, Chandler MJ, ForemanRD. Propriospinal neurons in the C1-C2 spinal segments proj-ect to the L5-S1 segments of the rat spinal cord. Brain ResBull 1998;47:43-7.
32. Arkuszewski Z. Involvement of the cervical spine in backpain. Man Med 1986;2:126-8.
33. Andersson GBJ, Lucente T, Davis AM, Kappler RE, Lip-ton JA, Leurgans S. A comparison of osteopathic spinalmanipulation with standard care for patients with low backpain. N Engl J Med 1999;341:1426-31.
34. Grostic JD. Upper cervical care and functional leg length in-equality. Proceedings of the Sixth Annual Conference on Re-search and Education. 1991 June 21-23; Monterey, California.San Jose (CA): Consortium for Chiropractic Research; 1991.p. 70-3.
35. Grostic JD, DeBoer KF. Roentgenographic measurement ofatlas laterality and rotation: a retrospective pre and postmanipulation study. J Manipulative Physiol Ther 1982;5:63-9.
36. Reinert OC, editor. Chiropractic procedure and practice. Flo-rissant (MO): Marian Press; 1976. p. 78-95.
37. Downe JW, editor. Technique manual of Life College, School ofChiropractic. Marietta (GA): Life University; 1993. p. 14-34.
38. Hinson R, Brown S. Supine leg length differential estimation:an inter- and intra-examiner reliability study. Chiropr Res J1998;5:17-22.
39. Hi nson R, Pfleger B. Pre- and post-adjustment supine leg-length estimation. J Chiropr Educ 2000;14:37-8.
40. Walsh P. Physicians’ desk reference. 55th ed. Montvale (NJ):Medical Economics; 2001. p. 1929, 2716, 3252.
41. Jayson MIV. Outcome measures for back pain: introduction,justification, and epidemiology. In: Erhlich GE, Khaltaev NG,editors. Low back pain initiative. Geneva: World Health Or-ganization; 1999. p. 8-12.
42. Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P,Goldsmith CH. Reliability of pain scales in the assessmentof literate and illiterate patients with rheumatoid arthritis.J Rheumatol 1990;17:1022-4.
43. McCormack HM, Horne DJ, Sheather S. Clinical applicationsof visual analogue scales: a critical review. Psychol Med 1988;18:1007-19.
44. Scott J, Huskisson EC. Vertical or horizontal visual analoguescales. Ann Rheum Dis 1979;38:560.
45. Baker DJ, Pynsent PB, Fairbank JCT. The Oswestry DisabilityIndex revisited: its reliability, repeatability and validity, and acomparison with the St Thomas Disability Index. In: RolandMO, Jenner JR, editors. Back pain: new approaches torehabilitation and education. Manchester, England: Manches-ter University Press; 1989. p. 174-86.
46. Fairbank JCT, Couper J, Davies JB, O’Brien JP. The OswestryLow Back Pain Disability Questionnaire. Physiotherapy 1980;66:271-3.
47. Stratford PW, Binkley J, Solomon P, Gill C, Finch E. Assess-ing change over time in patients with low back pain. PhysTher 1994;74:528-33.
48. Hedlund JL, Vieweg BW. The Zung Self-rating DepressionScale: a comprehensive review. J Oper Psychiatry 1979;10:51-64.
49. Lambert MJ, Hatch DR, Kingston MD, Edwards BC. Zung,Beck, and Hamilton rating scales as measures of a treatmentoutcome: a meta-analytic comparison. J Consult Clin Psychol1986;54:54-9.
50. Main CG, Wood PLR, Hollis S, Spanswick CC, Waddell G.The distress and risk assessment method: a simple patientclassification to identify distress and evaluate the risk of pooroutcome. Spine 1992;17:42-52.Hoiriis et alJournal of Manipulative and Physiological TherapeuticsChiropractic, Medical Care for Back PainVolume 27, Number 6397
Page 10
Page 10
51. Tanaka-Matsumi J, Kameoka VA. Reliabilities and concurrent
validities of popular self-report measures of depression, anxi-
ety, and social desirability. J Consult Clin Psychol 1986;54:
328-33.
52. Dequeker J, Panayi G, Pinus T, Grahame R. Medical manage-
ment of rheumatic musculoskeletal and connective tissue dis-
ease. New York: Marcel Dekker; 1997. p. 41.
53. Evans RC. Schober’s test. In: Evans RC, editor. Illustrated
essentials in orthopedic assessment. St. Louis: Mosby; 1994.
p. 326-7.
54. Waterworth RF, Hunter IA. An open study of diflunisal, con-
servative and manipulative therapy in the management of low
back pain. N Z Med J 1985;98:372-5.
55. Bronfort G, Goldsmith GH, Nelson CF, Boline PD, Anderson
AV. Trunk exercise combined with spinal manipulative or
NSAID therapy for chronic low back pain: a randomized,
observer blinded clinical trial. J Manipulative Physiol Ther
1996;19:570-82.
56. Cherkin DC, Deyo RA, Battie M, Street J, Barlow W. A
comparison of physical therapy, chiropractic manipulation,
and provision of an educational bookl et for the treatment
of pati ents with low back pain. N Engl J Med 1998;339:
1021-9.
57. Balon J, Aker PD, Crowther ER, Danielson C, Cox PG,
O’Shaughnessy D, et al. A comparison of active and simulated
chiropractic manipulation as adjunctive treatment for child-
hood asthma. N Engl J Med 1998;339:1013-20.
58. Browning R, Jackson JL, O’Malle y PG. Cyclobenzaprine
and back pain: a meta-analysis. Arch Intern Med 2001;161:
1613-20.
59. Dopf CA, Mandel SS, Geiger DF, Mayer PJ. Analysis of spine
motion variability using a computerized goniometer compared
to physical examination. A prospective clinical study. Spine
1995;19:586-9.
60. Miller SA, Mayer T, Cox R, Gatchel RJ. Reliability problems
associated with the modified Schober technique for true lum-
bar flexion measurement. Spine 1992;17:345-8.
61. Williams R, Binkley J, Bloch R, Goldsmith CH, Minuk T.
Reliability of the modified Schober and double inclinometer
methods for measuring lumbar flexion and extension. Phys
Ther 1993;73:33-44.
62. Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van
Rompay M, et al. Trends in alternative medicine use in the
United States, 1990-1997. Results of a follow-up national sur-
vey. JAMA 1998;280:1569-75.
63. Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR,
Delbanco TL. Unconventional medicine in the United States–
prevalence, costs, and patterns of use. N Engl J Med 1993;328:
246-52.
64. Morin CM, Colecchi C, Brink D, Astruc M, Mercer J,
Remsberg S. How “blind” are double-blind placebo-controlled
trials of benzodiazepine hypnotics? Sleep 1995;18:240-5.
65. van Tulder MW, Koes BW, Bouter LM. Conservative treat-
ment of acute and chronic nonspecific low back pain: a sys-
tematic revi ew of rand omized controlled trials of the most
common interventions. Spine 1997;22:2121-56