
Is Autism a Brain Disorder or a Gut Disorder?
By Joan Fallon, D.C., DICCP
Recently autism has been in the news on a daily basis. With a large increase in the numbers of cases—one in 166 live births, as the most recent statistic—health authorities have undertaken significant studies related to the etiologies of autism. Characterized by multiple deficits in the areas of communication, development and behavior; autistic children are found in every community in this country and abroad. Recent findings point to a significant increase in autism, which cannot be accounted for by means such as misclassification. The state of California recently reported a 273 percent increase in the number of cases between 1987 and 1998. Estimates now hover around the four through 20 per 100,000 children. Recent findings from the MIND Institute at the University of California at Davis states that, ‘‘The unprecedented increase in autism in California is real and cannot be explained away by artificial factors, such as misclassification and criteria changes, according to the results of a large statewide epidemiological study.”
 Many causes of autism have been postulated, ranging from environmental and toxicological causes to genetics. The most current thinking including that of many members of the U.S. Congress and others is that vaccination, and specifically the mercury-based preservative in the vaccines, is causing brain damage in children resulting in autism. Conflicting findings have prevailed in the literature with respect to the potential of vaccines as a causative factor in autism. Certain findings, such as those of Andrew Wakefield, have pointed to a live measles virus in the GI tracts of children with autism. Some studies have confirmed his findings, others have disputed it. Further, there are many anecdotal reports of regressive autism following administration of one or more vaccinations. Other parents report developmental problems from birth pointing to autism.
Many causes of autism have been postulated, ranging from environmental and toxicological causes to genetics. The most current thinking including that of many members of the U.S. Congress and others is that vaccination, and specifically the mercury-based preservative in the vaccines, is causing brain damage in children resulting in autism. Conflicting findings have prevailed in the literature with respect to the potential of vaccines as a causative factor in autism. Certain findings, such as those of Andrew Wakefield, have pointed to a live measles virus in the GI tracts of children with autism. Some studies have confirmed his findings, others have disputed it. Further, there are many anecdotal reports of regressive autism following administration of one or more vaccinations. Other parents report developmental problems from birth pointing to autism.
Last year the author proposed, in a widely published paper, a mechanism by which the use of amoxicillin/clavulanate may be a possible contributing factor in the causation of autism. Administered liberally since 1989, Augmentin as it is known in the U.S. began being cited in the literature for Otitis Media in 1989. During the manufacture of Augmentin, a large buildup of urea is common. The nitrogen poses a potential explosive component and the potential for nitrogen/urea poisoning of the GI system exists in children treated with Augmentin.
Most likely, autism has multiple etiologies with environmental and genetics causes all playing a role in the etiology. Whether vaccine or medication induced, other toxins or allergens as a factor, the etiology of autism continues to be uncertain.
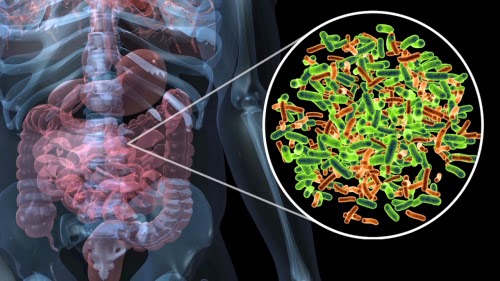
Gastrointestinal Factors
In 1989, Horvath from the University of Maryland proposed that a child with autism who received an endoscopy had significant changes occur with respect to his autism. Determined that the factor involved was the administration of secretin which was used to detect stomach tumors during the endoscopic procedure, secretin was proposed as a potential treatment for autism. Having mixed findings with respect to the potential efficacy of secretin, the debate still rages in many quarters of the autistic community. During that time certain mechanisms were discussed as to why the secretin could potentially be efficacious. It was determined by the author that potentially certain toxins such as vaccines and or antibiotics such as Augmentin could injure the lining of the small intestine. Augmentin of course has long been known to cause GI irritation, and Wakefield’s findings of measles in the small intestines could potentially set the child up for GI dysfunction.
 Injury to the lining of the small intestines could injure the secretory cells in the lining. The secretory cells of the small intestine among other things respond to the pH change in the small intestine. A bolus of food from the stomach enters the small intestine at a pH of 1 or close to 1. This acidic bolus triggers the secretory cells of the small intestine to send out the hormone secretin. The secretin, which is a neuropeptide, reaches the pancreas which responds by sending out zymogens which are the precursors to the digestive enzymes as well as bicarbonate ions. The zymogens are sent out by the pancreas to prevent autolysis of the pancreas itself that could happen in the presence of activated enzymes.
Injury to the lining of the small intestines could injure the secretory cells in the lining. The secretory cells of the small intestine among other things respond to the pH change in the small intestine. A bolus of food from the stomach enters the small intestine at a pH of 1 or close to 1. This acidic bolus triggers the secretory cells of the small intestine to send out the hormone secretin. The secretin, which is a neuropeptide, reaches the pancreas which responds by sending out zymogens which are the precursors to the digestive enzymes as well as bicarbonate ions. The zymogens are sent out by the pancreas to prevent autolysis of the pancreas itself that could happen in the presence of activated enzymes.
The bicarbonate ions change the pH of proximal small intestines to approximately a 6.4 pH. The zymogens are then converted into active enzymes. Trypsinogen changes to trypsin which then in turn converts the chymotrypsinogen to chymotrypsin and so on. These changes can only take place in the presence of the secretin activation.
Mechanism of Action
If the small intestine or pancreas itself is injured through the use of medications such as Augmentin, or from vaccination or other insult, it is likely that the secretin mechanism is unavailable or disrupted. For example, if the secretin mechanism is altered due to injury to the lining of the small intestines by the urea/nitrogen residue from Augmentin, then the entire pH change cannot take place. If the pH change does not occur then the conversion of the inactive to the active forms of the digestive enzymes does not occur.
The face of the lack of conversion of the enzymes, incomplete or absent digestion of certain foodstuffs can and will occur. So for example, if a lipase or protease such as chymotrypsin is not converted from chymotrypsinogen to chymotryspin, or the pancreas does not manufacture sufficient amounts of the enzymes, incomplete protein digestion will occur. In the case of an incomplete or absent digestion of a fat or a protein, the molecule of undigested protein for example, remains in the small intestines and can act as an allergen. This allergen can act as a toxin to the body and produce buildup of certain substances, which are further toxic to the body.
In the case of fats, undigested fats can become rancid and cause a toxic buildup in the body. The rancid fats can create an allergic irritation or act as a poison. This is the idea which has been referred to as “leaky gut syndrome.”
By definition, “leaky gut syndrome” is a change in the permeability of the intestinal lining to large macromolecules such as those of undigested fats and proteins which generally comes from an inflammation or other change or damage to the mucosa of the small intestine. Further, if there is damage to the small intestinal lining, then the IgA (immunoglobulin A) present in that lining can be injured and absent, allowing pathogens to enter which otherwise would not be there.
The presence therefore of allergens, and pathogens can upset the balance to further allow other things such as yeast overgrowth to occur.
So, What Does the Brain Have To Do With It?
If we examine the fact that the GI system in autistics is affected by these conditions, and there is a lack of digestion, the brain can be significantly affected. In the first few years of life, and especially under the age of 2 years, the brain is in demand for growth. The largest growth in the brain takes place during these first few years, and if not given the building blocks necessary for that growth, the brain will be at a severe disadvantage.
If protein digestion is not taking place, then the proper number and amounts of amino acids will not be present to make other proteins. The body therefore must prioritize the use of the available amino acids, and it is possible or at least theoretical that the body will sacrifice the use of the available amino acids to allow the most function not necessarily the highest function. The same is true of the digestion of fat. If the proper fat digestion is not taking place, then there is going to be a dearth of formation of myelin and other fat necessary structures in the body.
The allergens, which can result from the lack of fat and the lack of protein digestion can therefore lead to autism.
 Gastrointestinal Markers of Autism
Gastrointestinal Markers of Autism
The examination of autistic children is difficult under the best of circumstances. Due to their significant sensory issues, obtaining blood and urine samples are difficult, especially in the child as young as 2.
Examination of the stool therefore is a far more easy method of obtaining a biological sample.
When examining the potential for GI markers for autism it is important to look for those markers which keep within the physiology of the above hypotheses. If there is a potential for a lack of protein digestion, measuring the levels of chymotrypsin could potentially be a marker for this problem. If the secretory cells are damaged there could potentially be a lack of secretin in the blood stream as a result of the pH 1 in the small intestines. Without the pH change from 1 to 6.4 in the small intestines, the chymotrypsinogen never is converted to chymotryspin and the level of chymotryspin therefore should be extremely low should the hypothesis be a good one. Measuring fecal chymotrypsin has long been done in those children with cystic fibrosis (CF) for they too have pancreatic involvement and a lack of enzymes to digest food. Indeed all CF patients take digestive (pancreatic) enzymes when they eat.
Further if there is a condition in the small intestines whereby the lack of digestion allows for an imbalance and the presence of other pathogens, examining for those pathogens could be another helpful examination in determining autism. The presence of these pathogens, as measured by their antigenic presence could also be used as an early marker for regressive autism.
Examination of the diets of these children will reveal an interesting aversion to protein. These children generally have diets laden with carbohydrates and very little protein. This is most likely the body’s adaptation to an inability to digest protein.
Fecal Chymotrypsin
Fecal chymotrypsin was measured in 10 children. Fifty children with Autism and 50 age matched controls who are not autistic, or exhibit autistic behaviors. The autistic children were confirmed through the use of a CARS test (Childhood Autism Rating Scale). Fecal chymotrypsin is measured with normal being greater than 8.4. The results are as follows in FIGURE 1:
The means of the two samples are significantly different, and meet the criteria for statistically significant findings. The use of fecal chymotrypsin is therefore an important tool to examine the potential need for protein digestion in the children with autism. Where N=100 for the total subjects, the mean for the autistics is 3.1, and for the non-autistics 24.6.
Pancreatic (Digestive Enzymes)
Thirty-one autistic and 31 non autistic children had their chymotrypsin levels measured. In FIGURE 2. 13 of the autistic children who had abnormal fecal hymotrypsin were administered pancreatic (digestive) enzymes including a protease, lipase and an amylase for 30 days. The results demonstrate a significant change in the level of fecal chymotrypsin in FIGURE 3.
Elevation of the fecal chymotrypsin levels was seen throughout the study, across all subjects.
Conclusion
There are many issues, which can be examined with respect to the etiology of autism. While the etiology is probably multi-factorial, there has never been a biological marker for autism. Whether from a spat of chronic ear infections for which the allopath prescribed numerous antibiotics or from a vaccine, which produces regressive autism, the GI system of the child is likely damaged based upon the common GI marker findings.
It is important to look at the entire child, and an important part of their workup should be a GI marker test, which is commercially available. If damage has been done by outside intervention such as antibiotics or vaccination, it is possible that the child will require replacement with pancreatic (digestive) enzymes.
This study is not intended to examine the full range of scientific data surrounding these findings but rather to give the practitioner an introduction to potential biological findings in the child with autism.
Dr. Joan Fallon is a member of the ICA Pediatrics Council Board of Directors and is the Immediate Past Council Chair. She has been recognized for her autism research and was awarded a patent for her enzyme therapy treatment by the U.S. Patent and Trademark Office. Dr. Fallon is a full-time practitioner in New York.
References
Malhotra S, Gupta N. Childhood disintegrative disorder. Reexamination of the current concept. J Am Acad Child Adolesc Psych 2002;41(10):1239–45.O’Callaghan FJ. Autism – what is it and where does it come from?. QJM 2002;95(5):263–5.Wing L, Potter D. The epidemiology of autistic spectrum disorders: is the prevalence rising. Ment Retard Dev Disabil Res Rev 2002;8(3):151–61.Croen LA, Grether JK, Selvin SJ. Descriptive epidemiology of autism in a California population: Who is at risk? Autism Dev Disord 2002;32(3):217–24.Fallon, J. Could one of the most widely prescribed antibiotics amoxicillin/clavulanate “augmentin” be a risk factor for autism?Med Hypotheses. 2005;64(2):312-5.D.J. Weber, N.E. Tolkoff-Rubin and R.H. Rubin, Amoxycillin and potassium clavulanate: an antibiotic combination. Mechanism of action, pharmacokinetics, antimicrobial spectrum, clinical efficacy and adverse effects, Pharmacotherapy 4 (1984) (3), pp. 122–136.University of California, Davis, MIND Institute (October 2002). Report to the Legislature on the Principal Findings from the Epidemiology of Autism in California: A Comprehensive Pilot Study. MIND Institute web site:http://mindinstitute.ucdmc.ucdavis.edu.Claudio L. NIEHS investigates links between children, the environment, and neurotoxicity. Environ Health Perspect 2001;109(6):A258–61.Wakefield AJ. Enterocolitis, autism and measles virus. Mod Psych 2002;7(Suppl 2):S44–6.N. Akshoomoff, K. Pierce and E. Courchesne, The neurobiological basis of autism from a developmental perspective, Dev Psychopathol 14 (2002) (3), pp. 613–634.I. Rapin, The autistic-spectrum disorders, New Engl J Med 347 (2002) (5), pp. 302–303.J. Hallmayer, E.J. Glasson, C. Bower, B. Petterson, L. Croen and J. Grether et al., On the twin risk in autism, Am J Hum Genet 71 (2002) (4), pp. 941–946.H.J. Boermans, Diagnosis of nitrate toxicosis in cattle, using biological fluids and a rapid ion chromatographic method, Med Hypoth. 16 (1985) (1), pp. 61–64.J.W. Tyler, Cot-death: the ammonia factor, Med Hypoth. 6 (1985) (1), pp. 61–64.I. Brook and K. Shah, Effect of amoxycillin with or without clavulanate on adenoid bacterial flora, Chemotherapy 48 (2001) (2), pp. 269–273.L. Tazi-Lakhsassi, A. Abid and M. Sehlane, Tolerance of amoxicillin–clavulanic acid combination in the child, J Int Med Res 14 (1986) (3), pp. 158–161.C.D. Bluestone, Modern management of otitis media, Pediatr Clin North Am 36 (1989) (6), pp. 1371–1387.K.H. Chan, E.M. Mandel, H.E. Rockette and C.D. Bluestone et al., Comparative study of amoxicillin-clavulanate and amoxicillin. Treatment of otitis media with effusion, Arch Otolaryngol Head Neck Surg 114 (1988) (2), pp. 142–146.C.D. Marchant, P.A. Shurin, C.E. Johnson, D. Murdell-Panek, J.C. Feinstein and D. Fulton et al., A randomized controlled trial of amoxicillin plus clavulanate compared with cefaclor for treatment of acute otitis media, J Pediatr 109 (1986) (5), pp. 891–896.RX List. Retrieved September 12, 2002 Available from: http://www.rxlist.com.I.S. Bennett et al., 6-(Substituted methylene) penems, potent broad spectrum inhibitors of bacterial B-Lactamse. V. chiral 1,2,3-triazolyl derivatives, J Antibiot. 44 (1991) (9), pp. 969–978.Shoichet T, et al. United States Patent No. 6,448,238. Washington, DC: US Patent and Trademark Office; 2002.Weston R, Shoichet T. Abstracts of the Interscience Conference on Antimicrobial Agents and Chemotherapy, vol. 37; 1997 p. 80 [Abstract No. 1998:112776].C. Stevens, N.G. Kennaway and J.H. Fellman, Ammonia intoxication: a hazard during rehabilitation of protein-deprived rats, J Nutr 105 (1975) (11), pp. 1384–1390.G. Fricke, M. Doerck, D. Hafner, R. Horton and M. Kresken, The pharmacokinetics of ticarcillin/clavulanate acid in neonates, J Antimicrob Chemoth 24 (1989) (Suppl B), pp. 111–120.







