The mnemonic term SOAP – Subjective Objective Assessment Plan – was devised as a way for doctors to document their patient’s progress. Keeping the meaning of each letter in mind ensures your SOAP notes checklist is thorough and complete. It’s essential to standardize your SOAP notes for each patient, so that the records are easily understood by any healthcare provider. SOAP notes aren’t necessarily long, but they must contain all the information required, so that you can easily evaluate the patient’s progress over time. Medicare requires specificity in SOAP notes, and you can use the Medicare requirements for every patient in your practice.
SOAP NOTES CHECKLIST
Your SOAP notes must include:
• Vital signs
• Weight and height
• Patient’s subjective view of their pain and/or improvement
• Examination of patient and findings
• Assessment – this may include any applicable diagnoses
• Any laboratory results
• Imaging tests results
• Patient response to treatments
• Adjustments made
• Future planning treatment
For an initial consultation, your SOAP notes are longer than for subsequent visits. The Subjective section includes taking the patient’s complete history. After that, you need only report how the patient’s pain and condition have changed. That initial visit is generally when you will order a full range of tests, so the Objective of the SOAP section is less likely to bear repeating on later visits, although much depends on the individual patient.
SOAP NOTES PROTECT YOU
While every aspect of SOAP notes are important, there are some that can make a real difference if you are ever faced with a lawsuit. Your SOAP notes also play a part if you are audited and must justify your charges.
CHIROTOUCH AND SOAP NOTES
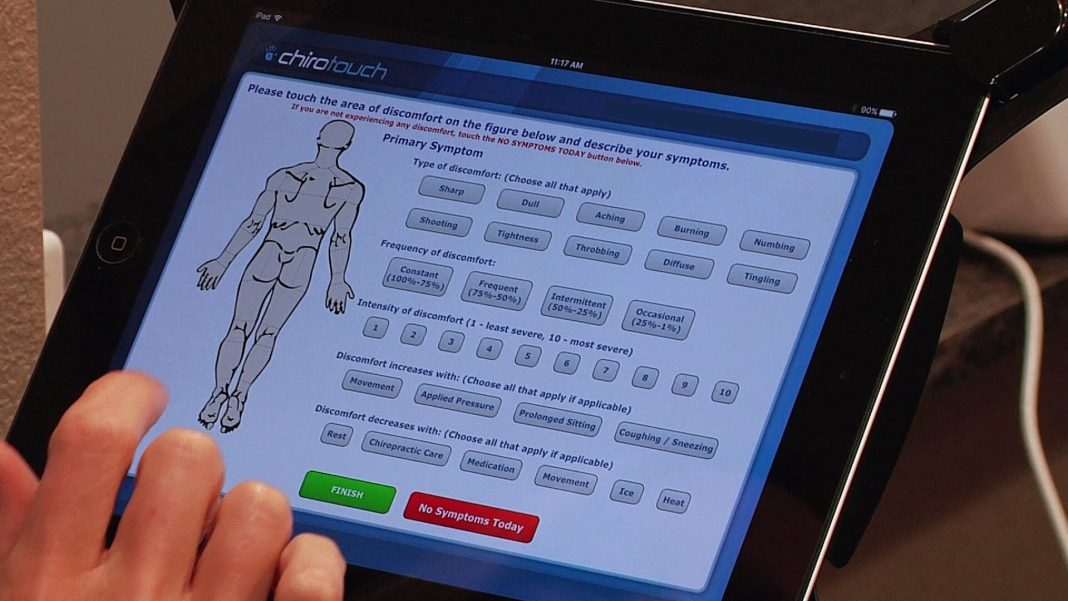
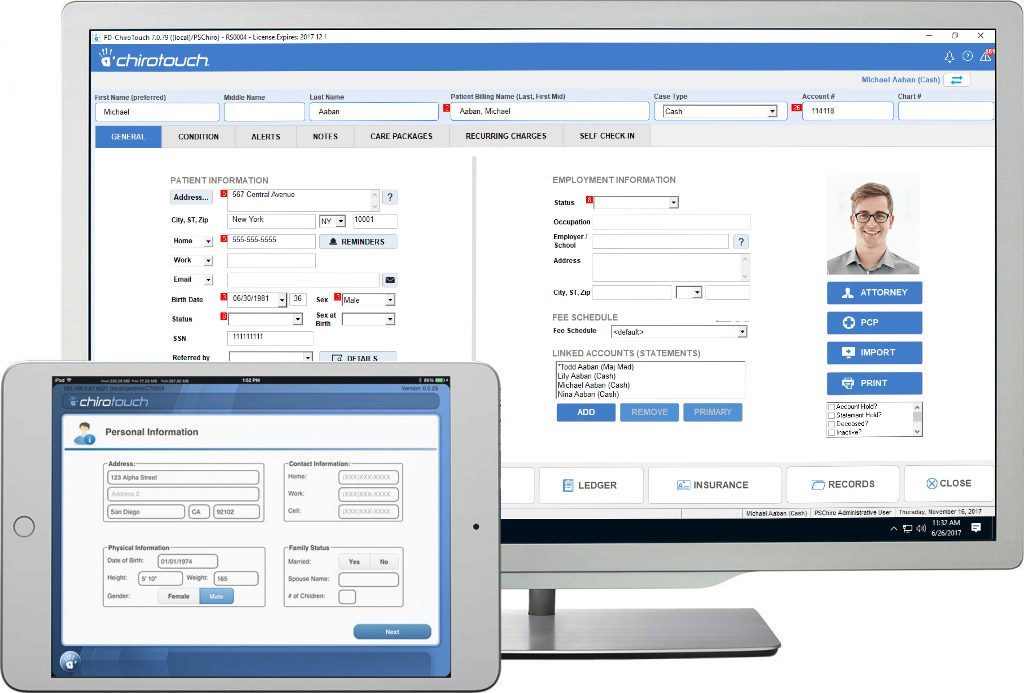
SOAP notes are crucial when it comes to evaluating treatment effectiveness. Good documentation allows you to make the proper treatment changes, when necessary. With ChiroTouch, you can ensure that your SOAP notes are standardized, so you won’t leave information off your checklist.