Plantar fasciitis: a condition in which weight-bearing stress irritates and inflames the tough connective tissues along the bottom of the foot. Like stated by Mary Biancalana in our blog post titled Plantar Fasciitis? Maybe Not, So Don’t Ice It!, most often, when pain is felt in the bottom of the foot, it is instantly diagnosed as plantar fasciitis. Since it is important to get an accurate diagnosis, it is important to correctly diagnose plantar fasciitis before treating. So, have you been properly diagnosed? Let’s learn more and how to treat plantar fasciitis!
Pathology
Plantar fasciitis develops when repetitive weight-bearing stress irritates and inflames the tough .png?t=1485892901051&width=331&name=calf_stretch(gastrocnemius).png) connective tissues along the bottom of the foot. High levels of strain stimulate the apo-neurosis to try to heal and strengthen. When the biochemical strain continues, it overwhelms the body’s repair capacity, and the ligaments begin to fail. This tear/repair process causes the chronic, variable symptoms that eventually can become unbearable for some patients.
connective tissues along the bottom of the foot. High levels of strain stimulate the apo-neurosis to try to heal and strengthen. When the biochemical strain continues, it overwhelms the body’s repair capacity, and the ligaments begin to fail. This tear/repair process causes the chronic, variable symptoms that eventually can become unbearable for some patients.
Since the plantar fascia inserts into the base of the calcaneus, the chronic pull and inflammation can stimulate the deposition of calcium, resulting in a classic heel spur seen on a lateral radiograph. Unfortunately, there is no correlation between the resence of a heel spur and plantar fasciitis, since many heel spurs are clinically silent, and most cases of plantar fasciitis do not demonstrate a calcaneal spur. 1
Examination
Biomechanical evaluation may find either excessive pronation or supination. The flatter, hyperpronating foot overstretches the bowstring function of the plantar fascia, while the high-arched rigid foot places excessive tension on the plantar aponeurosis. In either case, the combination of improper foot biomechanics and excessive strain causes the connective tissue to become inflamed. A careful assesment of the weight bearing alignment of the lower extremeties is helpful, since many patients will have funactional imbalances in the kinetic chain, into the pelvis and spine.
Direct palpation of the plantar fascia will demonstrate discrete painful areas, most commonly at the insertion on the anterome-dial calcaneus.2 Fibrotic thickenings are frequently felt- these are remants of the repetitive tear and repair process. With the foot relaxed, grasp the toes and gently pull them up into passive dorsiflexion. Since this maneuver stretches the irritated plantar aponeurosis, it is frequently quite painful, which is an obviously positive objective sign.
Treatment
Acute Relief 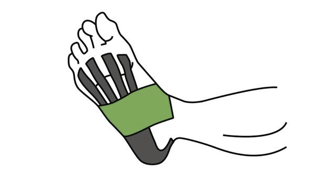
• Taping: temporary of support for the strained plantar fascia can be provided with figure-eight taping or with low-dye strapping
• Restricted activity: repetitive and straining activities should be strictly limited, intiaially. Immobilization is not recommended.
• Cryotherapy: Ice massage and/or cold packs help reduce pain and inflammation.
Healing
• Ultrasound: Initially pulsed, then constant and direct (once inflammation has subsided).
• Transverse friction massage: to stimulate blood flow and collagen deposition.3
• Vitamin C with bioflavonoids: a natural anti-inflammatory that can speed healing
Adjustments
• Calcaneus: Reduction of the calcaneus posteririty to relieve sagittal stress. Kell’s technique uses a posterior-to-anterior thrust on a table with a pelvic drop piece.4
• Other foot joints: Brantingham found various areas of joint dysfunction in the tarsal and metatarsal koints in patients with plantar fasciitis.5 The navicular and first metatarsophalangeal joints are often involved.
Orthotic Support
• Orthotics for pronation: to support the arches and reduce the stress on the plantar fascia
• Orthotics for supination: arch support with added visco-elastic material to cushion the foot and decrease the amounf of shock at heel strike.
• Heel spur correction: A “divot” in the surface of the material under the heel to spread pressure away from the fascial insertion.
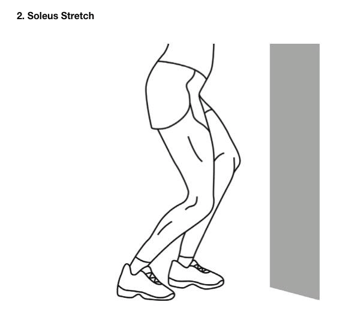
• Heel and foot stretching: “Runner’s stretch” for the calf and the bottom of the foot.
• Intrinsic muscle strengthening: Toe curl excercises (while sitting, gather a towel on the floor up under the arch, and repeat three times).
• Extrinsic muscle strengthening: Toe raises (while standing on the edge of a stai, slowly rise up on balls of feet) and ankle stabilizing series with tubing
Plantar fasciitis usually responds well to focused, conservative treatment. Steroid injections and surgical release are seldom necessary and are best avoided. One of the most important treatment methods is to reduce any tendency to pronate excessively. In addition to custom-fitted orthotics, runner should wear well-designed shoes that provide good heel stability. The use of corrective orthotics can prevent many overuse problems from developing in the lower extremeties. Investigation of foot biomechanics is a good idea for all patients but especially those who are recreationally active.
This blog was curated from the article titled “Plantar Fasciitis” by John K. Hyland, DC, DACBR, DABCO, CSCS and was published in the magazing The American Chiropractor Volume 38, Number 11, 2016.
References:
1. Lapidus PW, Guidotti FP. Painful heel: report of 323 patients with 364 painful heels. Clun Orthop 1965;39;178.
2. Subotnick SI. Sports medicine of the lower extremity. New York; Churchill Livingston; 1989:237.
3. Lear L. Transverse friction massage. Sports Med Update 1996;10:18-25.
4. Kell PM. A comparative radiologic examination for unresponsive plantar fasciitis. J Manip Physiol Therap 1994;17:329-34.
5. Kibler WB, et al. Functional rehabilitation of sports and musculoskeletal injuries. Gaithersburg, MA: Aspen Publishers; 1998:280.
Tags: plantar fasciitis