Functional medicine is rapidly gaining traction (pardon the pun) among chiropractors, but can chiropractors legally practice functional medicine? Let’s look at definitions of functional medicine as well as scope of practice issues faced by non-MD healthcare practitioners.
Functional Medicine Practice
More and more physicians are leaving primary care and opening a specialized medical practice in functional medicine.
Meanwhile other professionals–such as chiropractors, and even psychologists–are looking to functional medicine as a way to help patients (and also develop new revenues lines and avenues of professional satisfaction).
What is “functional” medicine?
According to the Institute for Functional Medicine:
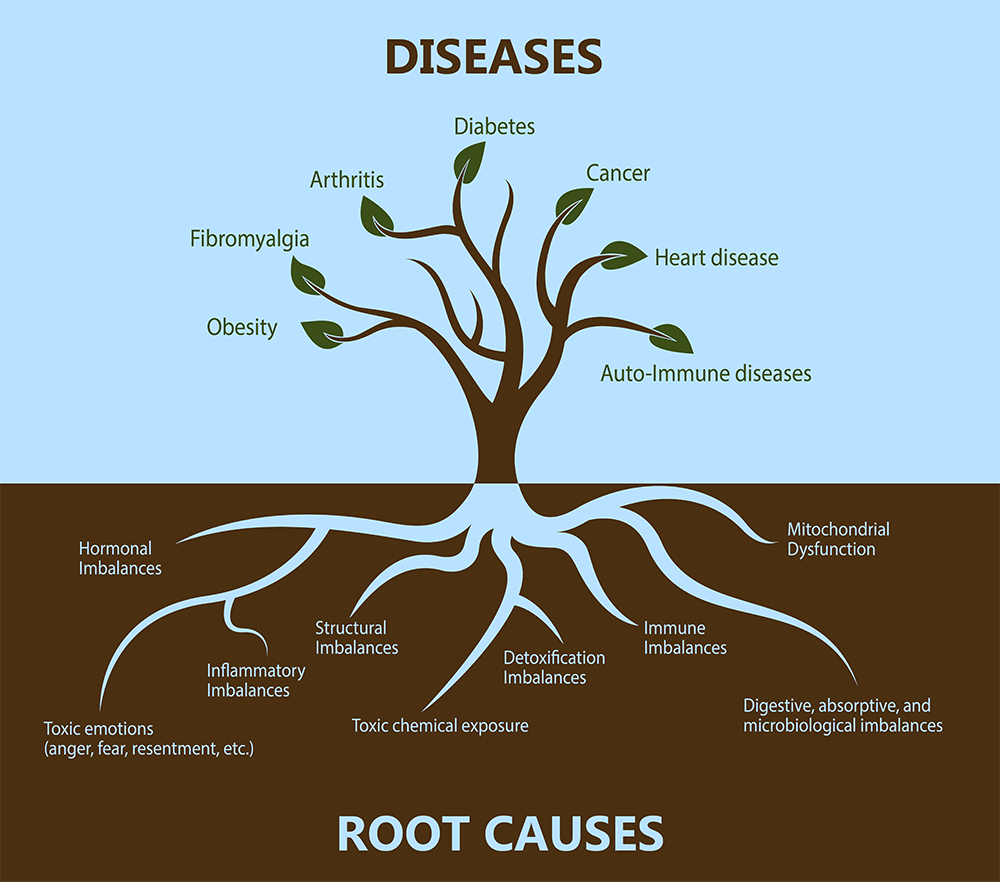
Functional medicine addresses the underlying causes of disease, using a systems-oriented approach and engaging both patient and practitioner in a therapeutic partnership. It is an evolution in the practice of medicine that better addresses the healthcare needs of the 21st century. By shifting the traditional disease-centered focus of medical practice to a more patient-centered approach, functional medicine addresses the whole person, not just an isolated set of symptoms. Functional medicine practitioners spend time with their patients, listening to their histories and looking at the interactions among genetic, environmental, and lifestyle factors that can influence long-term health and complex, chronic disease. In this way, functional medicine supports the unique expression of health and vitality for each individual.
This sounds a lot like integrative medicine, with its emphasis on a systems-oriented approach, therapeutic partnership, patient-centered approach, the whole person and not just symptoms, unique expression of health and vitality.
More specifically, though, the above definition of functional medicine emphasizes “the interactions among genetic, environmental, and lifestyle factors that can influence long-term health and complex, chronic disease.”
Whether or not patients understand the emphasis and branding of functional medicine, functional medicine is increasingly popular among clinicians.
Medical Malpractice and Medical Board Discipline
Our law firm recently conducted a website review for a physician opening a functional medicine practice.
This physician already had her consent forms prepared by another healthcare attorney, but she wanted to be sure her website didn’t unduly expose her to risk of medical malpractice or medical board discipline.
One of the issues with online marketing is that practitioners (and companies) can make aggressive therapeutic claims that run afoul of various legal rules (for dietary supplements companies, FDA and FTC rules; but for practitioners, rules governing advertising, laws against unfair business practices, or whatever else plaintiff lawyer trolls or aggressive boards can find in an investigation).
For years, from a risk management perspective, we’ve emphasized using two defenses to medical negligence:
- assumption of risk by the patient (within reason)
- respectable minority
In one version of assumption of risk, the patient and physician contract for a different
style of medicine than the usual community approach. This is not necessarily a deviation from standard of care–simply a different therapeutic approach.
As to the “respectable minority,” no one knows exactly what is considered “respectable” or why it rhymes with bespectacled; but with the gathering popularity of functional medicine among more and more sizable physician segments, one can argue that the respectable minority is present.
Some of the decision points we discussed with our functional medicine physician included:
- disclaiming primary care and agreeing with the patient to enter into a specialist medical role
- requiring the patient to designate a primary care physician of record
- using clear consent forms to document a robust informed consent process
- following some of the ground rules laid out by the Federation of State Medical Boards in its Guidelines on Use of Complementary and Alternative Medical Therapies by Physicians
- using evidence-based approaches and documenting the literature supporting therapeutic approaches
- evaluating safety and efficacy of chosen therapies and selecting the ones with the best benefit/risk ratio
Negligence can lead to both a malpractice lawsuit and medical board discipline, so reviewing the website for claims and language, as well as paying attention to the other risk management strategies, is critical.
For more information, see our post, 4 Legal Tips for Setting Up a Functional Medicine Practice.
Practice of Functional “Medicine” by Chiropractors, Psychologists, and Other Practitioners
There’s an inherent problem when non-medical doctors advertise and practice functional medicine, in that the word “medicine” is included and only medical doctors (and DOs) can practice “medicine.”
Analyzing scope of practice in detail is important.
For example, we reviewed some law in Texas about chiropractic scope of practice and found an Attorney General Opinion from 2000, which asked:
Does the Chiropractic Practice Act, as amended in 1999, permit doctors of chiropractic to order and receive the results of diagnostic testing from licensed medical laboratories, including urinalysis, arthritis panel, urine count, glucose tolerance test male-female endocrine profile, standard blood profile (CBC with differential) and pregnancy testing?
The AG likes to ask yes/no questions in this way.
We also reviewed the statutory definition of chiropractic:
… the science and art of locating and removing interference with nerve transmission and nerve function. A chiropractic physician diagnoses and treats neuromuscular and musculoskeletal conditions through physical agent modalities and manipulative therapies. The adjustment, manipulation or treatment shall be directed toward restoring and maintaining the normal neuromuscular and musculoskeletal function and health of the patient. A chiropractic physician will also make appropriate health referrals for conditions that may not be treated by physical agent modalities and manipulative therapies. Patient care shall be conducted with due regard for nutrition, environment, hygiene, sanitation and rehabilitation designed to assist in the restoration and maintenance of the patient’s health. Nothing in this chapter shall be construed to authorize the chiropractic physician to practice any branch of medicine osteopathy, as defined in chapters 6 and 9 of this title, or surgery, including venipuncture or the prescribing of medication, acupuncture being the exception.
We added some bold for emphasis. Here, the statute is clear, and as we’ll discuss below, the AG read it straight.
A Narrower Scope of Practice
No matter what the state, almost always the additional caveat exists, prohibiting the chiropractor (or other non-MD) from practicing “medicine.”
Put simply: If it ain’t chiropractic, it’s medicine!
The reason is that medical doctors have unlimited licensure to diagnose and treat disease, whereas other practitioners have limited licensure as defined by their scope of practice, which is inherently narrower.
As the AG opinion put it, citing a Texas court:
the field of chiropractic [is] limited to the treatment of those illnesses and diseases of the human body which doctors of chiropractic reasonably believe can be aided by the manual manipulation of the spine. On the other hand, the field of doctors of medicine covers all human illnesses and diseases and their diagnosis, treatment and prevention.
The ground is clear: chiropractors, limited; on the other hand, medicine, covers all human illnesses and diseases and their diagnosis, treatment and prevention.
If you want to change this, Option A is: lobby legislatures to change the rules of the regulatory landscape for medicine and chiropractic so that the whole limited/unlimited licensure concept bubbles away.
Or option B:
- Buy a time machine
- Go back to the 1800s and challenge the AMA’s political dominance and influence over health care legislation; or create an alternate timeline in which the ACA (American Chiropractic Association) is ascendant.
Note: I am in the middle of Terminator Genisys so Option B seems plausible.
The Texas AG concluded that Texas law “did not change the established principles regarding the scope of chiropractic practice with regard to diagnostic testing so as to permit doctors of chiropractic to order and receive the results of diagnostic testing from licensed medical laboratories, including urinalysis, arthritis panel, urine count, glucose tolerance test,male-female endocrine profile, standard blood profile (CBC with differential) and pregnancy testing.”
The AG did bat the question to legislative lobbying:
We think additional legislation is required before chiropractors may order and receive from licensed medical laboratories the results of the diagnostic tests.
Re-Brand
I do have another suggestion, in case there’s a run on time machines and stock is temporarily out. That is: re-brand.
The legal definition of medicine is typically broad and historically, chiropractors, acupuncturists, massage therapists, naturopathic physicians, and other practitioners have had to battle in the state legislatures for their own licensure or for exemptions and carve-outs, enabling them to practice.
It you are a chiropractor practicing functional medicine, then in addition to having your attorney review scope of practice issues relevant to your practice, you might rebrand what you’re doing as functional health, not medicine.
Language means a lot to regulators and enforcement authorities.
As lawyers, we’re wordsmiths. Attention to language is what we do. Many times, what’s required is to titrate marketing vs. compliance. Neither is all-or-nothing. The more aggressive the marketing, the greater the risk of regulatory enforcement; conversely, the tighter and more thoroughly the compliance, the less room for edgy marketing.
Legal compliance is really about understanding the rules and playing the edge so that 21st business models can have the right legal boundaries under rule systems that essentially arose in prior centuries.
In the case of FDA law for dietary supplements, cosmetics and medical devices, we only have to go back to the 20th century, but for medical licensure we’re in the late 19th.
Questions about your functional medicine practice? Contact us. In this timeline, astute legal counsel can navigate the ship to shore.
 Michael H Cohen – Founder Michael H Cohen – Founder |
The Michael H Cohen Law Group provides healthcare legal and FDA and FTC legal (and regulatory) counsel to health technologies and products (medical devices, cosmetics, and dietary supplements to wearable tech and virtual reality (VR) devices), healthcare ventures (MSOs to telemedicine, medical apps, and machine learning), and health & wellness practices and centers (medical groups to medical spas).Our legal team offers expertise in corporate & transactional legal services, healthcare regulatory & compliance advice, and healthcare litigation and dispute resolution, in cutting-edge areas such as telemedicine, mobile and virtual health. Founder Michael H. Cohen is a keynote speaker on healthcare law and FDA law. |